In Chicago, along the Dan Ryan and Kennedy expressways, it is normal to be greeted by the homeless holding up signs for help. Many have turned the underbelly of I-94 into their makeshift homes. Upon closer examination, people holding signs can readily be assessed to be homeless, unemployed or drug dependent, but many suffer from the battles of mental illness. These are the obvious among us, but there are many among us; hidden in the workplaces and classrooms – independently functioning in the shadows of normalcy.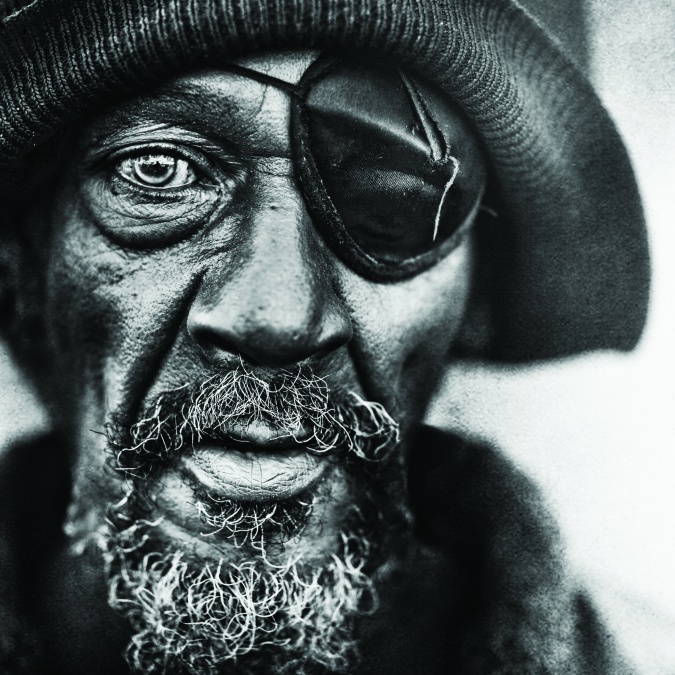
In the last twenty years, we’ve witnessed victims of fatal shootings at schools in Columbine, Denver, Sandy Hook, Connecticut, Virginia State Tech and most recently Umpqua College in Roseburg, Oregon. In many of these cases, the alleged shooter, typically a young white male, is deemed to be suffering from some type of mental illness according to main stream media accounts.
We often wonder what drives a person to commit such heinous acts of violence. Yet, whenever there is a murder or shooting committed in Chicago by Black or Hispanic men, it is almost never linked to mental illness, no matter the circumstances. As the Cook County Jail population exploded, it seemed to include more cases that involved individuals that suffered from some form of mental illness.
Mental Illness it is often a topic that has been avoided in Black households for generations: whether out of embarrassment, lack of financial assistance, proper healthcare or shame—it has become a slow and silent killer in our community. What’s in the dark must now come into the light.
According to the National Alliance on Mental Illness (NAMI), one in every five adults in the U.S. experiences a mental health condition and one in every five children ages 13-18 have or will experience the same. However, within the Black community the numbers concern 18.6% of Black Americans compared to 19.3% of White Americans dealing with a mental health condition according to a race study conducted in 2012.
Six mental health care clinics closed in 2012 by the City of Chicago in predominately Black communities that included Auburn Gresham, Back of the Yards, Beverly/Morgan, Northtown/Rogers Park, Northwest, and the Woodlawn neighborhoods. Therefore it’s no surprise to see the recent uptick in panhandling throughout the city.
The state-run mental health facility, Tinley Park Mental Center, also suffered serious budget cuts when their hospital was closed in 2012 under Governor Pat Quinn without much warning, displacing patients with few alternative solutions. Lydia Healthcare located in Robbins, Illinois is a for-profit clinic that has felt the increase of patients as a result of budget cuts to the regional health care system. CEO, Susan Simonsen, has owned and operated the 412 bed clinic, which employs 160 staffers since her father purchased the building 25 years ago and housed mostly seniors at the time. Eventually it converted into a full-service mental rehabilitation clinic.
 Being a solid presence in the South Suburbs for many years, Ms. Simeonsen states that, “With the closings of the mental health agencies, family members are starting to bring family members to the emergency room, which will stop soon because we are working with Managed Care. Managed Care providers are telling us that we need to keep people out of the hospital and have them stabilized here. I’m fine with that but if they are in a crisis, I can’t have them here because we’re not a ‘crisis stabilization’ facility. I can have a crisis unit but it costs more money than the State is paying us. So, it’s always a vicious cycle.”
Being a solid presence in the South Suburbs for many years, Ms. Simeonsen states that, “With the closings of the mental health agencies, family members are starting to bring family members to the emergency room, which will stop soon because we are working with Managed Care. Managed Care providers are telling us that we need to keep people out of the hospital and have them stabilized here. I’m fine with that but if they are in a crisis, I can’t have them here because we’re not a ‘crisis stabilization’ facility. I can have a crisis unit but it costs more money than the State is paying us. So, it’s always a vicious cycle.”
Since, the facility is not controlled by the State or County administrators, they often accept what they prefer to call ‘consumers’ not ‘patients’ without the pressure of payment. Often they receive people that have either gone off of their medication(s) and require stabilization to be restored to functionality. Also there are cases where family members have been hurt in some way and seek the clinic as a last resort. The stigma that this carries with some African American families when a loved one is suffering from mental instability –depression, bipolar syndrome, or schizophrenia is either ignoring the behavior or replacing it with a faith base remedy.
Further, often the mentally ill, seek means outside of medical help and fall into drugs, alcohol and deviant behavior oftentimes appearing as an individual who is wild, when all the while their behavior is manic or schizoid. Their indulgence is an attempt to bring them balance. Being aware of what mental illness symptoms look like is key in being able to seek help for yourself or loved ones.
Ronald Robinson, Community Relations Director at Lydia Mental Healthcare is also a parent whose son suffered a brain injury in an automobile accident, noticed an immediate change in his mental stability. Robinson said, “My son bounced around from five different facilities. Everyone in my family said, ‘Bring that boy home, he’ll be alright. We can pray over him, he’s not crazy.’ He came here to Lydia for six months but now he’s living independently. He will always have challenges but he’s still here and able to take care of himself.”
Praying away the illness is what some of us heard was the remedy for those with mental issues when growing up. Because of the stigmas that were associated with mental illness—touched, a little slower than others, knocking out the demons Blacks deny it when they recognize the behavior. The unfamiliarity of how to cope can put further pressure on those without knowledge and proper education of helping friends and loved ones. In many cases, as seen by the Cook County justice system it’s often too late to prevent a crime by a person experiencing mental instability until they are incarcerated.
According to Cook County Sheriff, Tom Dart – the county jail is the largest mental health facility in the country with 30 percent occupancy held by inmates that are in need of mental health treatment. Bukky Mitchell, an Admissions Director for Lydia Healthcare, who worked with his of- fice in the past and is currently working to assist with the mentally ill population, states, “There are so many people that are far gone mentally that when you are sitting with in-mates for a short period, you know something is not quite right. By the time we are called, inmates are high risk,” Mitchell said. “In the State of Illinois if a person is rated high risk’, we are required to provide a private room. If we don’t have any available, guess where they end up? Back on the streets or in the jails again.”
In 2015, Health & Disability Advocates (HDA) conduct- ed a review of the Community Health Needs Assessments (CHNAs) which was completed by Chicago hospitals required by the Patient Protection Affordable Care Act (ACA). In parts of the review, socio-economic factors contributed to making treatment options less available to African Americans. According to the U.S. Census Bureau, as of 2012, 19% of African Americans have no form of health insurance. Although, the Affordable Care Act is making it easier and more affordable to get insured, most clinics still rely on Medicaid to cover low-income patient’s expenses.
Also in the report were some concerns by the State’s review of Chicago’s Department of Public Health’s performance on submitting payment claims which are required to be submitted to IDHD in order to be reimbursed for services rendered. In 2013, Chicago’s score on submissions to be reimbursed decreased to 52 percent, and from May 2014 to May 2015, it dropped to a dismal 26 percent. The states requirement is that providers maintain a 70 percent billing submission rate and when it falls below 50 percent, there is a suspension of Medicaid payments. In order to be reinstated, a Plan of Correction is required and must be supported by either another on-site review or desk audit that demonstrates improvements are occurring according to the HDA review.
This can also mean CDPH’s mental health clients are not receiving the standard and necessary care and that staffing may not be adequately paid thereby jeopardizing the overall quality standards that providers are required to have when joining these health care systems.
When the City closed six mental health centers in mid- 2012, it simultaneously awarded $500,000 in funding to seven agency partners to increase community capacity for psychiatry services for uninsured persons. The funded agencies are: Community Counseling Centers of Chicago (C4), Human Resources Development Institute (HRDI), Lutheran Social Services of Illinois (LSSI), Metropoli- tan Family Services, Mt. Sinai Hospital, Pilsen Wellness Center and Thresholds. An eighth partner, Mercy Hospital and Medical Center, was also funded when an additional $500,000 was awarded in 2013, and again in 2014.
Upon review of the City of Chicago 2015 Budget proposal, there is an effort to expand the school-based health centers that serve Chicago students –13 centers out of the 30 SBHC centers. We reached out to Mayor Emanuel’s office as to how many of these health centers are located in predominately African American communities and will they include mental health services for people? Budget spokesperson, Molly Poppe said, “By 2019, the City plans to open five more school-based health centers through strategic investments of e-cigarette tax revenue and TIF funds. Each new center will provide comprehensive primary care and mental health services,” Poppe said, “The location of the new school-based health centers have not yet been identified, but the City will choose locations in low-income communities that are medically underserved as defined by census data and other federal data.”
As the State budget stalemate continues to stretch the needs in underserved communities gripped with this silent and gradual killer in the African American community, advocates such as a NAMI is providing necessary education to the community.
 The statistics provided showed that 10.3% of Black females and 6.6% of Black males will use Mental Health services compared to 21.5% White Females and 11.3% White Males with even a lower number of Hispanic females 9.2% and Hispanic males 5.5%. So, while more people have signed up under the Affordable Healthcare Act and others qualify for Medicaid assistance—the challenge in the African American community is recognizing the need for mental health treatment.
The statistics provided showed that 10.3% of Black females and 6.6% of Black males will use Mental Health services compared to 21.5% White Females and 11.3% White Males with even a lower number of Hispanic females 9.2% and Hispanic males 5.5%. So, while more people have signed up under the Affordable Healthcare Act and others qualify for Medicaid assistance—the challenge in the African American community is recognizing the need for mental health treatment.
Part of the problem is the cultural disconnection among African Americans refusing treatment due to a lack of African American mental health professionals. Only 3.7% of members in the American Psychiatric Association and 1.5% of members in the American Psychological Association are African American.
What will it take before we pay close attention to the behaviors of those close to us that raise red flags? And, why is it considered ‘normal’ to occasionally ‘snap off’ on a girlfriend, boyfriend, family member or through social media when the lines of venting or letting off steam is acceptable in our society? When are the lines crossed and how do we properly identify what is acceptable and what is a cry for help? In society, where unruliness in the classroom can lead to either immediate discipline or childhood medication—critics believe there is still a cultural and educational disconnect in our Black community.
Regardless, assistance beyond the home, school and church in receiving professional care is vital to make the correct psychiatric analysis for those living with mental health challenges. It is not ‘their’ problem, it is ‘our’ problem. The stigma of therapy being a ‘rich’ and White problem or economic burden is not the case with community base centers there to assist. Our community must take the necessary steps to acknowledge the problem, seek help and accept and work with the outcome, which in the end can save a life.